Anatomy
The bones of the knee joint include the femur (thigh bone), tibia (shin bone) and patella (kneecap). The articular surfaces are covered with a few millimetres of cartilage that serves to reduce stress on the articular surfaces. The kneecap slides against the femur when the knee bends and extends.
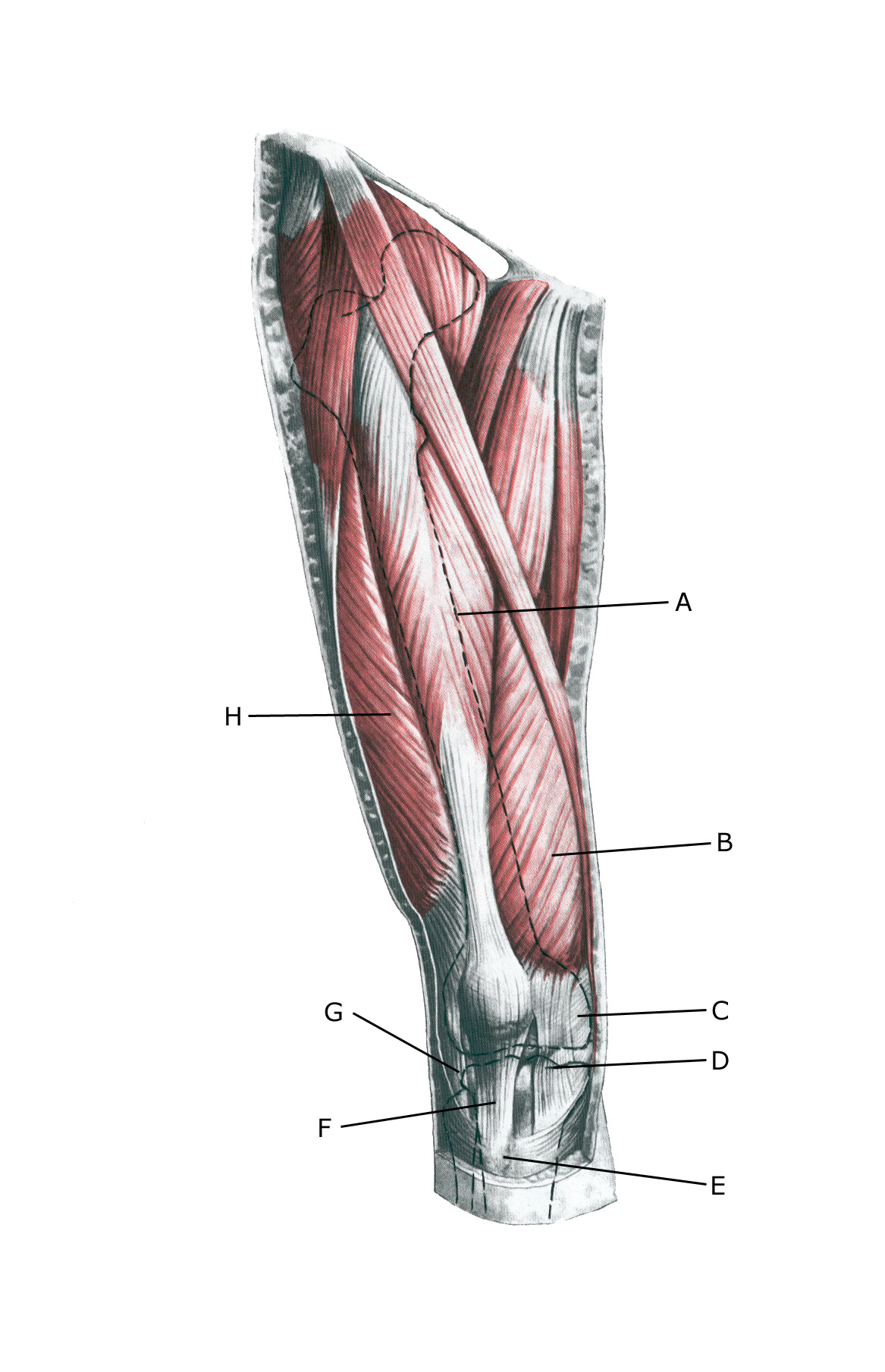 Knee from the front:
Knee from the front:
A. M. rectus femoris
B. M. vastus medialis
C. Retinaculum patellae mediale
D. Retinaculum patellae mediale
E. Tuberositas tibiae
F. Lig. Patellae
G. Retinaculum patellae laterale
H. M. vastus lateralis
Cause
Repeated repetitive repetitive strain of the patellar tendon in football, handball (running, jumping, kicking), for example, causes an overload-related inflammation (‘inflammation’) at the attachment of the patellar tendon to the growth zone (apophysis) on the lower edge of the kneecap (Sinding-Larsen disease).
The damage is caused by the load exceeding what the growth zone can withstand.
Training load should be reduced during periods of rapid growth (measure the height of young athletes every 3 months). Training should generally be varied and avoid repetitive movements. Alternate between different exercises over time to reduce strain. Quality of training is more important than quantity.
Symptoms
Slow onset tenderness in 9-15 year olds at the patellar tendon attachment on the lower edge of the kneecap during and after sports activity. Symptoms fade at the latest when the growth zone closes around the age of 17.
In some (few) cases, there may be persistent symptoms beyond the teenage years if the bone changes in the growth zone are significant, which can lead to strain-related tendon problems in adulthood.
Examination
Usually, the diagnosis can be made by general clinical examination alone with the detection of localised pressure tenderness on the patellar tendon attachment on the lower part of the kneecap.
If there is any doubt about the diagnosis, the changes are detected with an ultrasound scan. See ultrasound scan.
Treatment
Treatment primarily involves relief from pain-inducing activity (jumping, kicking) and anterior thigh muscle stretching (Corbi F, et al. 2022), and is exactly like Osgood-Schlatter treatment. If treatment is started quickly, in some cases the injury can heal in a matter of weeks. It is therefore crucial to respond to the first symptoms to avoid prolonged periods of injury.
It is important that the athlete, parents and coach are informed, understand and respect the need for load management during the rehabilitation period in order to avoid long-term injuries that can last six months to a year (Longo UG. et al., 2016 ).
If the pain has been present for several months before responding, the relief period can be very long (six months to a year). It is usually sufficient to refrain from the most strenuous exercises (jumping) during the relief period, while many other training exercises can be performed without discomfort.
In the vast majority of cases, it will therefore still be possible to participate in parts of the sports activity together with your friends. As with all overuse injuries to the growth zones, vigorous strength training of the injured tendon attachment is generally not indicated, as the growth zone cannot be trained stronger.
Gentle activity that prevents muscle wasting (atrophy) is recommended. Later, muscle training can be slowly escalated within the pain threshold (Rathleff MS, et al. 2020). Once the pain has subsided, sporting activity can be gently resumed. Relapses will often occur, after which relief should be resumed as soon as possible.
The ice treatment can be repeated every time tenderness is induced at the patellar tendon attachment during the rehabilitation process. Adrenal cortical hormone injections usually have no place in treatment. In general, there is little evidence for the effectiveness of various treatment recommendations (Midtiby SL, et al. 2018).
Bandage
Some people find that applying tape or a similar bandage around the tibia just below the kneecap can relieve the discomfort, see tape.
Complications
The prognosis is very good (but can be long-lasting) and the injury usually does not cause any discomfort later in life. Failure to do so should be considered:
- Cartilage damage in the joint
- Anterior knee pain
- Meniscus lesion
- Osgood-Schlatter as well as fractures and infections.
Only in very rare cases has a tear of the lower edge of the patella where the patellar tendon attaches been described. The torn bone part (where the patellar tendon attaches) can be screwed to the tibia in a simple operation with good results.
