Anatomy
The brain is surrounded by the meninges and protected by the skull bone.
Cause
During violent shaking, the brain can be impacted against the skull bone with such force that fluid extraction and haemorrhage occurs in the brain or on the surface of the brain. Autopsy studies have shown an increased incidence of neuropathological changes in the form of protein deposits in the brain among athletes in contact sports such as American football, rugby and soccer many years after they have stopped playing.
Similar protein deposits are also seen in neurodegenerative diseases such as Parkinson’s disease and Alzheimer’s dementia.
Symptoms
Headaches, dizziness, memory problems, sensitivity to light and sound, mood swings, difficulty concentrating, general malaise, nausea, visual disturbances, drowsiness increasing to remoteness, unconsciousness, seizures and in the worst cases death. In the rare cases where fatalities have occurred in sports after blows to the head, this often happens if two head injuries occur in the same match.
Examination
Any athlete who suffers a blow to the head and subsequently complains of discomfort should immediately stop the sporting activity and be examined by a medical professional. In cases of loss of consciousness, unconsciousness or balance problems, the athlete should be removed from the field and assessed by a doctor or other authorised medical professional and should not return to sporting activity on the day of the injury.
If a sideline assessment does not indicate a concussion, a healthcare professional can assess whether the athlete can continue the sporting activity. If the athlete is allowed to continue, a follow-up assessment must be made to determine if there is a delay in the development of symptoms.
If there is no doctor or other medical professional present, the athlete should be assessed at the local hospital if concussion is still suspected.
All head injuries must be taken seriously, as in some cases, life-threatening bleeding or chronic damage can occur.

Treatment
For acute head trauma, the primary focus should be on potentially life-threatening conditions such as brain haemorrhage, seizures and skull or spine fractures, and acute treatment should be directed towards these, including seeking the appropriate emergency medical attention to manage these conditions.
For non-acute treatment needs, rest and relief and refrain from physical and cognitive (thinking) activity until symptoms have subsided. Taking painkillers to continue sporting activity is not recommended and can be risky.
Before physical activity can be resumed, there must be no ongoing physical, cognitive or emotional symptoms or sleep disturbances. Abstinence from alcohol and caffeinated drinks is advised.
By gradually increasing activity levels, the goal of returning to normal daily activity is achieved for most adults within two weeks and for children within four weeks. If the symptoms have not subsided after 14 days, a (renewed) medical examination and possibly a neuropsychological examination is advisable. If the discomfort has not subsided after 14 days, a (repeat) medical examination and possibly a neuropsychological examination is advisable.
The strongest prognostic factor for how quickly you will be symptom-free after a sports-related concussion is the severity of the symptoms in the the first few days after the injury. Few symptoms in the first day after injury is a favourable prognostic indicator.
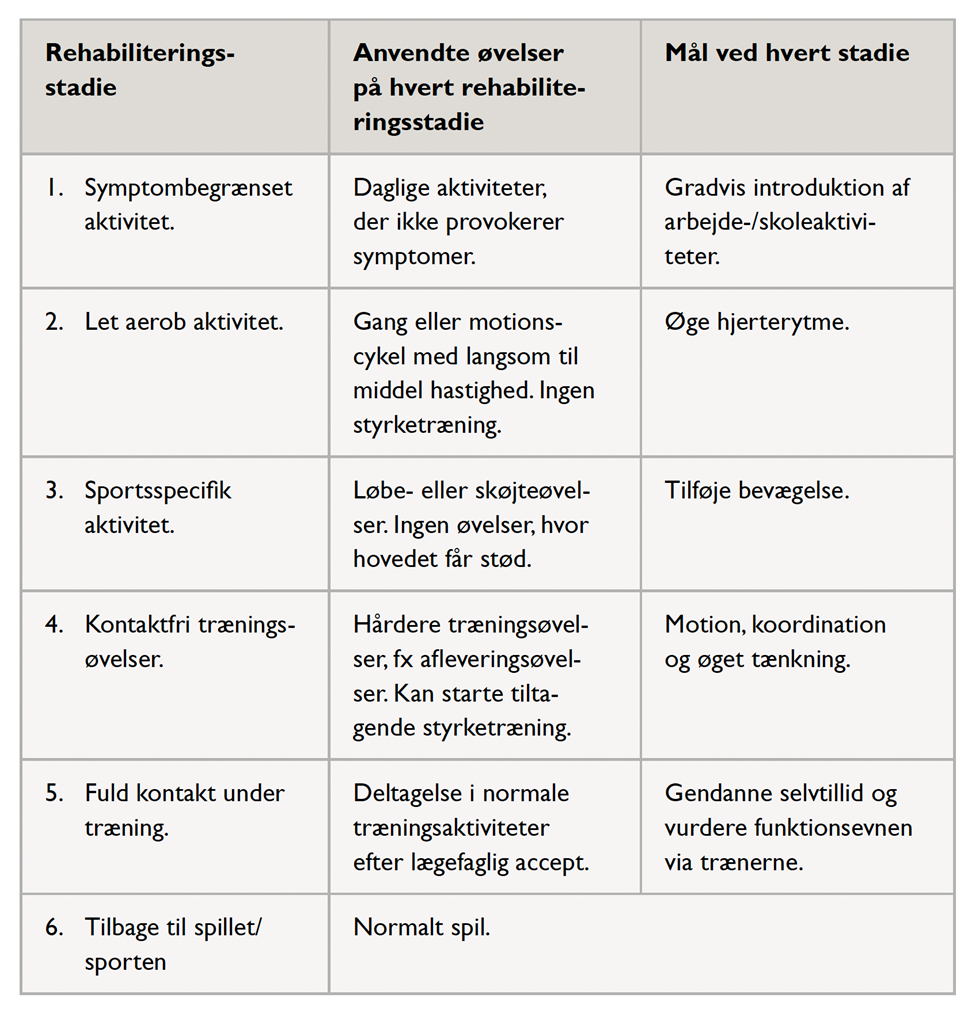
Rehabilitation, specific:
Relief and rest for 1-2 days. After this, training can be gradually resumed according to the figure without worsening symptoms. At least 24 hours should pass between each of the 6 steps.
Especially
More widespread use of helmets in different sports will undoubtedly reduce the number of concussions and their consequences.
