Anatomy
There are numerous bursae around the shoulder joint that serve to reduce pressure on muscles, tendons and ligaments where they lie close together and against bony prominences.
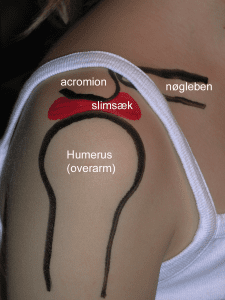
Between the upper bony prominence of the shoulder blade (acromion) and the upper scapular muscle (M supraspinatus) lies the shoulder’s largest bursa (bursae subacromiale), which can communicate with the shoulder joint.
Cause
With repetitive strain, often with the arm over the shoulder, the bursae can become ‘inflamed’ (inflamed), produce increased fluid, swell and become painful. Although the condition is called mucosal ‘inflammation’, it is an irritation and there is usually no infection in the mucosa.
When the arm is abducted, the supraspinatus muscle and bursa slide under the upper bony prominence of the shoulder blade (acromion), where the bursa and supraspinatus tendon can become pinched (impingement) between the acromion and the humeral head (caput humeri).
Shoulder bursitis is often combined with tendonitis of the upper scapular muscle (and impingement) and the treatment is the same. Osteoarthritic changes on the underside of the AC joint and degenerative changes in the supraspinatus tendon increase the risk of impingement.
In some cases, for unknown reasons, acute calcification of the mucosa (bursitis calcarea) can occur, causing very severe acute pain.
Symptoms
Pain in the shoulder, often radiating into the upper arm. The pain worsens when the arm is moved away from the body and above head height. Mucosal inflammation often causes pain at night and pain when lying on the side where the inflamed bursa is.
Examination
The diagnosis is usually made on general clinical examination, where there is pain when lifting the arm, especially between 80-120 degrees (positive pain arc). Various clinical examinations can be conducted that do not always allow a definite diagnosis. If there is any doubt about the diagnosis or lack of progress, an ultrasound scan should be performed early on to diagnose and assess the severity by detecting thickening and possible fluid in the mucosa, blood vessel growth (Doppler activity)
See ultrasound scan of shoulder with thickened mucosa with Doppler activity (colours)
See ultrasound scan of shoulder with thickened mucosa with acute calcification
Treatment
Treatment primarily includes relief from pain-inducing activity, stretching and gradual rehabilitation of the muscles around the shoulder within the pain threshold. Gene training can be supplemented with anti-inflammatory drugs (NSAIDs) or injection of adrenal cortex hormone into the mucosa (Papalexis N, et al. 2022). If rehabilitation and medical treatment are ineffective, surgical treatment with removal of the bursa and part of the acromion (subacromial decompression) can be tried (Horowitz EH, Aibinder WR. et al. 2023).
This reduces the risk of the supraspinatus muscle and the bursa getting pinched between the head of the humerus (caput humeri) and the upper bony projection of the shoulder blade (acromion) when the arm is lifted.
Rehabilitation
Usually, once the pain has subsided, sporting activity can be gently resumed, especially if you have been able to identify a triggering cause that has subsequently been removed. In general, gentle training of the shoulder muscles is recommended, primarily with the arm below head level.
Complications
If the progress is not smooth, you should consider whether the diagnosis is correct or if there are complications.
In particular, the following should be considered:
- Rupture of the upper shoulder blade muscle
- Inflammation of the tendon sheath of the upper shoulder blade muscle
- Rupture of the biceps tendon
- Luxation of the shoulder joint
- Luxation of the joint between the shoulder blade and the collarbone
- Frozen shoulder
- Muscle infiltrations
- Meniscus lesion in the shoulder
- Nerve entrapment on the back of the shoulder blade
