Anatomy
The calf muscle (M. Gastrocnemicus) consists of two muscle heads that come together in a broad tendon band that continues into the Achilles tendon. Another large calf muscle (M. Soleus) attaches to the front edge of the Achilles tendon and forms part of the Achilles tendon. The Achilles tendon thus consists of the 3 calf muscles (Triceps Surae). The Achilles tendon attaches to the heel bone (calcaneus). Just in front of the Achilles tendon attachment to the heel bone is a mucous sac.
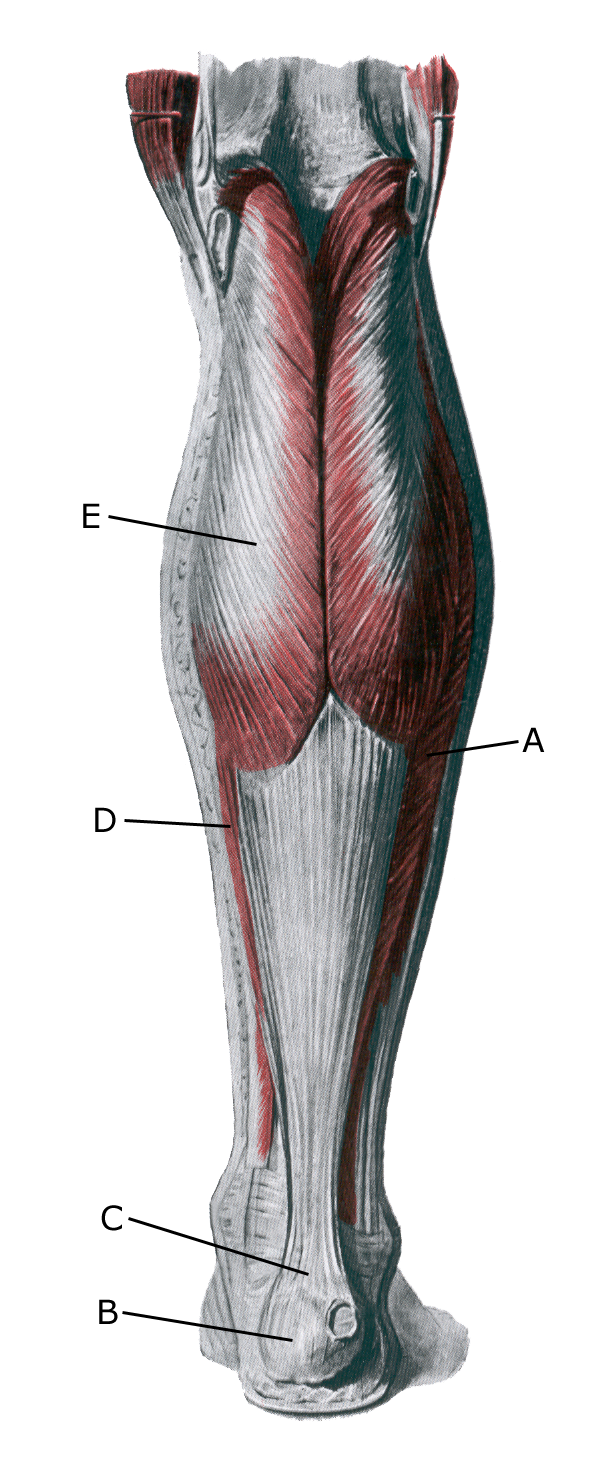 Lower leg from behind:
Lower leg from behind:
A. M. soleus
B. Tuber calcanei
C. Tendo calcaneus (Achillis)
D. M. gastrocnemius
Cause of the problem
“Inflammation” of the Achilles tendon occurs with repeated overuse, often in the form of running and pushing off. The risk of strain injuries to the Achilles tendon increases with age. The vast majority of cases of inflammation (tendinitis) of the Achilles tendon are localized 3-6 cm above the heel bone attachment and less frequently at the heel bone attachment (enthesitis), where it is often combined with bursitis.
The changes can be caused by wear and tear changes in the tendon (tendinosis). In recent years, the condition has been called Achilles tendinopathy regardless of whether the cause is inflammation (tendinitis) or wear and tear (tendinosis). Tendinopathy increases the risk of partial and total ruptures.
Symptoms
Pain when activating the Achilles tendon (running and pushing off), pressing on the tendon and stretching the tendon. The tendon often feels thickened. Symptoms can last for several years in some cases.
Examination
For slow onset tenderness/pain without sudden worsening, the diagnosis is made by clinical examination. For prolonged symptoms, lack of response to offloading and rehabilitation, and in all cases where there is a throbbing or sudden stabbing pain in the tendon, you should be examined by an appropriate professional and have an ultrasound scan performed.
The ultrasound scan can detect the extent of changes in the tendon: tendon thickness, blood vessel growth in the tendon (Doppler activity) – see ultrasound scan, inflammation of the tendon (tendinitis), wear and tear changes in the tendon (tendinosis), calcifications in the tendon, inflammation of the tendon tissue around the tendon (peritendinitis), mucosal inflammation (bursitis) and (partial) ruptures.
Treatment
The treatment of overuse Achilles tendonitis consists primarily of relief from the pain-inducing activity (running), stretching and slowly increasing strength training within the pain threshold.
If treatment is started quickly, the Injury can sometimes heal in just a few weeks. If the pain has been present for several months and an ultrasound scan shows thickening of the Achilles tendon, a rehabilitation program over several months/half years is often required. Special emphasis is placed on strength training by activating the tendon while stretching (eccentric training) or slow heavy strength training (Beyer R, et al. 2015).
If offloading and rehabilitation are not successful, rehabilitation may be considered supplemented with medical treatment in the form of arthritis pills, NSAIDs or injection of adrenal cortex hormone around the thickened part of the tendon(Johannsen F, et al. 2018). As adrenal hormone injection is always part of a long-term rehabilitation of a severe, chronic injury, it is crucial that the rehabilitation process lasts for (at least) six months to reduce the risk of relapse and rupture.
Naturally, after a long-term injury, the tendon cannot withstand maximum load after only a short-term rehabilitation period. Six months of rehabilitation before maximum load (jumping, sprinting) is allowed is not unusual. See General, chronic tendonitis.
Bandage
Taping for Achilles tendon problems is of questionable value, but can be tried. See tape
Complications
If the progress is not smooth, a (repeat) ultrasound scan should be performed to rule out (partial) rupture of the Achilles tendon.
Few sports injuries have such a high risk of causing chronic, athletically debilitating problems as Achilles tendonitis. In the most severe cases, despite all attempts at treatment and rehabilitation, the injury will often lead to the cessation of sport.
Especially
As Achilles tendonitis is difficult to treat, it is of great importance to prevent the injury from (re)occurring. The principles of rehabilitation (Rehabilitation, general) should be followed to avoid rapidly increasing training loads at the start of the season, after injury periods or with new running shoes.
Ultrasound scans of asymptomatic athletes frequently reveal changes in the Achilles tendon that have been documented to increase the risk of developing Achilles tendonitis symptoms over the next 12 months (Fredberg U, et al. 2008). This means that preventive strength and flexibility training can is started before the injury causes symptoms.
Rehabilitation
Rehabilitation program
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
