Anatomy
On the outside of the outer femoral prominence (greater trochanter), many muscles attach to the buttocks and around the hip. Between the various muscle tendon attachments are mucosal sacs to reduce the strain on muscles and tendons when they slide over the bony prominence or against each other.
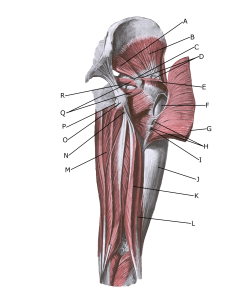 The gluteal muscles from behind:
The gluteal muscles from behind:
A. piriformis
B. gluteus minimus
C. Bursa m. piriformis
D. Bursae trochantericae m. glutei medii
E. gluteus medius (resectus)
F. Bursa trochanterica m. glutei maximi
G. gluteus maximus
H. Bursae intermusculares mm. gluteorum
I. Tuberositas glutea
J. Tractus iliotibialis
K. biceps femoris (caput longum)
L. biceps femoris (caput breve)
M. adductor magnus
N. subtendinea m. bicipitis femoris superior
O. Tuber ischiadicum
P. ischiadica m. glutei maximi
Q. gemilli sup. Et inf.
R. ischiadica m. obturatorii interni
Cause of the problem
With repeated strain or impact, the tendon attachments of the gluteal muscles on the outer femur (trochanter major) can become irritated – ‘inflamed’ (inflamed) and painful. The bursae between the tendons can also become irritated (bursitis). The pain on the outside of the hip is therefore often a combination of overloading of the tendon attachments and bursae.
In severe cases, the tendon fibres can rupture.
Symptoms
Pain when pressure is applied to the outside of the thigh, corresponding to the bursae and tendon attachments. The pain can radiate down the thigh and often into the buttocks, corresponding to the muscles related to the irritated bursa.
If the tendon attachments (gluteus medius and minimus) are ruptured, you are often unable to hold your hip up when standing on one leg (Tredelburg test).
Examination
In mild cases with only minimal tenderness, a medical examination may not be required. For more severe pain or lack of progress, an examination by a professional should be conducted to ensure proper diagnosis and treatment. Diagnosis is usually made by general clinical examination.
If the tendon attachments (gluteus medius and minimus) are ruptured, you are often unable to hold your hip up when standing on one leg (Tredelburg test).
If there is any doubt about the diagnosis or a suspected tendon rupture, an ultrasound or MRI scan can be performed.
It is not uncommon for the buttock and lower back disorder to be combined with mucosal inflammation at the outer femoral prominence (Zibis AH, et al. 2018) or MRI scans
Treatment
Treatment primarily includes relief from pain-inducing activity, stretching and graduated rehabilitation within the pain threshold. Of course, if the triggering cause is known, it should be removed. It is recommended to avoid sitting cross-legged, to avoid lying on the painful side and to sleep with a pillow between the legs when lying on the healthy side to reduce the stretch on the outside of the hip.
Treatment can be supplemented with anti-inflammatory drugs (NSAIDs) or injection of adrenal cortex hormone into the mucosa (Seidman AJ, et al. 2023).
As adrenal cortex hormone injection is part of a long-term rehabilitation of an often chronic injury, it is crucial that the rehabilitation programme lasts several months to reduce the risk of relapse.
Surgery is rarely indicated, but may be attempted in tendon attachment ruptures with significant discomfort without progress on other treatment (Lange J. et al 2024).
Complications
If the progress is not smooth, you should consider whether the diagnosis is correct or if complications have arisen:
In particular, the following should be considered:
