Anatomy
The muscles and tendons around the ankle joint are divided into 3 groups. A group at the front of the ankle (extensor tendons) that bend the foot up, a group behind the inside of the ankle (long flexor tendons) and a group behind the outside of the ankle (peroneal tendons) that help to stabilise and stretch the ankle. The tendons are partially embedded in tendon sheaths.
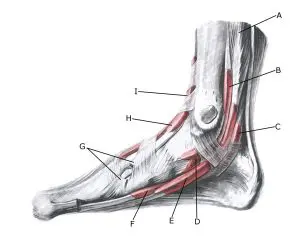
Foot, inner
A. M. flexor digitorum longus
B. Vagina synovialis tendinis m. tibialis posterioris
C. Vagina synovialis tendinis m. flexoris hallucis longi
D. Vagina tendinum m. flexoris digitorum pedis longi
E. Tendo m. tibialis anterioris
F. Vagina tendinis m. tibialis anterioris
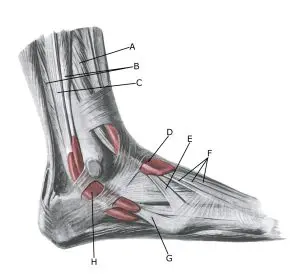 Foot, outer
Foot, outer
A. M. extensor digitorum longus
B. M. peroneus brevis
C. M. peroneus longus
D. Vagina tendinum m. extensoris digitorum pedis longi
E. M. peroneus tertius
F. Tendines m. extensoris digitorum longi
G. Vagina synovilis mm. peroneorum communis
Cause of the problem
Tendinopathy and tenosynovitis are either caused by mechanical irritation of the tendon and tendon sheath (e.g. from a shoe that is laced too tightly) or more frequently by repetitive stresses (hard landings, running with direction changes) that exceed the strength of the tendon and trigger an ‘inflammation’ of the tendon and/or tendon sheath.
The inflammation of the tendon can lead to a weakening and, in the worst case, rupture of the tendon. Usually it is the shock-absorbing muscles and their tendons behind (tibialis posterior) and in front of (tibialis anterior) the medial malleolus that are overloaded with the development of tendonitis and/or tendinitis.
Symptoms
In tendonitis and tendinitis, there is pain along the tendon that worsens with stretching and activation of the muscle. There is often the classic ‘pain triad’ with soreness at the start of exercise (‘difficulty starting’), improvement with movement and worsening with sustained exercise.
Examination
The diagnosis is usually made through a clinical examination. If there is any doubt about the diagnosis, an ultrasound scan can usually clarify this. Swelling of or along the tendon can often be seen and occasionally a crackling sensation (crepitation) is felt when the tendon is pressed with a finger. In severe cases, there is increased blood vessel growth in the tendon (Doppler activity).
Ultrasound scanning should be considered in all cases where there is no steady progress on offloading (Bordalo M, et al. 2023), see ultrasound scanning of tenosynovitis
Treatment
Treatment includes relief from pain-inducing activity, stretching and gentle rehabilitation of muscle strength within the pain threshold. Any pressure from shoes should be corrected. If no progress is made, you can try to supplement rehabilitation with medical treatment in the form of arthritis pills (NSAIDs) or ultrasound-guided injection of adrenal cortex hormone into the tendon sheath.
Complications
If the progress is not smooth, you should consider whether the diagnosis is correct or if there are complications:
In particular, the following should be considered:
