Anatomy
The bones of the wrist consist of 8 carpal bones (ossa carpi), which together with the 2 forearm bones (ulna) and radius (radius) form the wrist. There are also 5 metacarpal bones (ossa metarcarpi) and a total of 14 phalanges.
Wrist and wrist spine
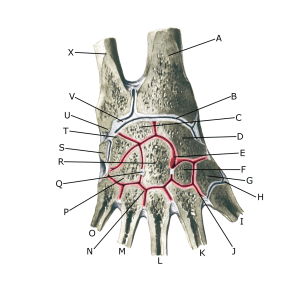
A. Radius
B. Articulatio radiocarpalis
C. Os lunatum
D. Os scaphoideum
E. Articulatio mediocarpalis
F. Os trapezoideum
G. Os trapezium
H. Articulatio carpometacarpalis pollicis
I. Ossa metacarpi I
J. Articulatio carpometacarpalis
K. Ossa metacarpi II
L. Ossa metacarpi III
M. Ossa metacarpi IV
N. Articulatio intermetacarpalis
O. Ossa metacarpi V
P. Os hamatum
Q. Lig intercarpale interosseum
R. Os capitatum
S. Os pisiforme
T. Os triquetrum
U. Processus styloideus
V. Discus articularis
W. —
Y. Ulna
Cause of the problem
Repeated strain can damage first the cartilage and then the bone under the cartilage (osteoarthritis). In some cases, the osteoarthritic changes can lead to ‘inflammation’ of the synovium (synovitis), which causes fluid formation, swelling, restricted movement and pain in the joint.
Osteoarthritic changes in the hand often occur after previous injuries (fractures, sprains). Osteoarthritic changes can be seen in the wrist itself and very frequently corresponding to the thumb root joint (articulatio carpometacarpale pollicis, CMC joint) as well as in the middle (PIP joint) and outer (DIP joint) joints of the fingers.
In osteoarthritis of the thumb root joint, there is often loosening of the ligaments due to osteoarthritis.
Symptoms
Pain, stiffness and jarring of the joint with movement and in the morning. Occasional swelling in the joint (synovitis). With osteoarthritis of the thumb root joint, there is often discomfort when gripping tweezers (when thumb and index finger are pinched together), trying to open jars, writing and turning keys in locks.
Examination
The diagnosis is made by clinical examination. It may be necessary to supplement this with an X-ray examination. Ultrasound and MRI scans can often show increased synovial fluid in addition to osteoarthritic changes.
Treatment
Reduction in activity that triggers pain. It is important to maintain mobility in the joint. Strength training of the muscles around the joint with osteoarthritis in the hand should be performed, but does not have the same proven positive effect as strength training of osteoarthritis in the large joints (e.g. hips and knees) (McGee C, et al. 2015).
There is no treatment that can restore the damaged cartilage (and bone). If there is swelling in the joint, you can try to reduce the inflammation of the synovium (synovitis) with NSAIDs or by draining the synovial fluid and injecting adrenal cortex hormone into the joint. Pain without joint swelling can be treated with paracetamol. For severe, painful osteoarthritic changes without sufficient effect of conservative treatment, surgery may be an option (Kloppenburg M, et al. 2019).
Rehabilitation
In general, exercises to maintain joint mobility and non-loading strengthening exercises for the muscles around the joint are advised (although evidence of the effect is limited).
Bandage
For osteoarthritic changes in the wrist and thumb, a bandage (orthosis) can be made to support and relieve the joint.
Complications
You should consider whether the swelling in the joint could be part of a generalised rheumatic disease.
