Anatomy
The bones of the knee joint include the femur (thigh bone), tibia (shin bone) and patella (kneecap). The articular surfaces of the femur, tibia and patella are covered with a few millimetres of cartilage that serves to reduce stress on the articular surfaces. Both inside and outside the joint there is an annular cartilage disc (meniscus). The knee joint is reinforced by a joint capsule that is laterally reinforced with an external and internal collateral ligament (ligamentum collaterale laterale and mediale). The medial meniscus attaches to the medial collateral ligament, while the lateral meniscus does not attach to the lateral collateral ligament.
Knee joint from the front:
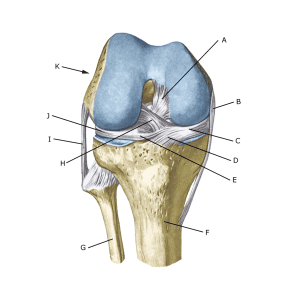
A. Ligamentum cruciatum posterius (Posterior cruciate ligament)
B. Ligamentum collaterale mediale/tibiale (Inner collateral ligament
C. Meniscus medialis (Inner meniscus)
D. Insertio anterior menisci medialis
E. Ligamentum transversum genus
F. Tibiae
G. Fibulae
H. Ligamentum cruciatum anterius (Anterior cruciate ligament)
I. Ligamentum collaterale laterale/fibulare (External collateral ligaments)
J. Meniscus lateralis (Outer meniscus)
K. Femur
Knee joints from above:
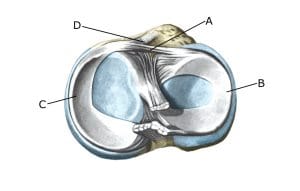
A. Ligamentum transversum genus
B. Meniscus lateralis (Outer meniscus)
C. Meniscus medialis (Inner meniscus)
D. Insertio anterior menisci
Cause of the problem
Acute meniscus tears usually occur when the knee is stretched while rotating. This squeezes the meniscus between the femur and tibia. Internal meniscus injuries are 3 times more common than external ones. Meniscus injuries in children are very rare.
The vast majority of meniscus ‘lesions’ are due to normal wear and tear that does not cause symptoms and therefore does not require treatment (Sihvonen R. et al 2013). Most meniscus lesions are thus comparable to ‘wrinkles in the skin’ – they affect image quality but are not a disease requiring treatment.
Symptoms
Pain on the joint line when pressing and rotating the knee. The pain often occurs suddenly with certain movements and may be accompanied by swelling in the knee. In some cases, the knee is felt to lock or fail (because a flap of the meniscus becomes trapped). In other cases, you may feel a small, tender swelling at the joint line (meniscus cyst).
Examination
Diagnosis can usually be made by clinical examination alone.
MRI and ultrasound scans can detect meniscus lesions (see picture), but often overdiagnosis of insignificant changes in the menisci that do not affect knee symptoms (Sihvonen R, et al. 2020).
Ultrasound scanning allows dynamic scans to be made while the knee is moving, making some hidden lesions visible. Video 1 (normal) and Video 2 (diseased).
Arthroscopy (binocular examination of the joint) can reveal many, but not all meniscus injuries.
Treatment
Treatment includes relief from pain-inducing activity and graduated rehabilitation of the knee within the pain threshold. Conservative treatment heals the vast majority of meniscus injuries (Sihvonen R, et al. 2020). If the discomfort does not slowly subside, or if it is obvious that the meniscus lesion is large or torn (e.g. assessed by MRI or ultrasound scan), surgery should be considered in younger patients.
Surgery can be attempted to stitch the torn meniscus piece (which will require a significantly longer rehabilitation period, but will probably reduce the risk of osteoarthritic changes in the knee in the long term). Acute injuries with a stretching defect in the knee and a suspected torn meniscus should be assessed and resolved within weeks. If the meniscus is torn from its attachment to the joint capsule, surgery with meniscectomy is advised.
Rehabilitation
After surgery, knee loading can start as soon as the pain and swelling in the knee have subsided. At best, full activity is possible after a few weeks. In uncomplicated cases, it should be possible to resume full sports activity within a month. The training should not cause increasing swelling (or pain) in the knee.
Complications
If no progress is made, you need to consider whether the diagnosis is correct. This will often require additional examinations (X-ray, ultrasound or MRI scan).
In particular, the following should be considered:
- Cartilage damage in the joint
- Rupture of the anterior cruciate ligament
- Rupture of the posterior cruciate ligament
- Synovial fluid in the popliteal space
- Inflammation of the mucous fold
As there is a risk of permanent injury, the injury should be reported to your insurance company
