Anatomy
 The large anterior thigh muscle (musculus quadriceps femoris) consists of four muscles (m vastus lateralis, m vastus medialis, m vastus intermedius and m rectus femoris). The muscles all attach together on the upper edge of the kneecap. The patellar tendon (ligamentum patellae) connects the lower edge of the kneecap to the upper, anterior part of the tibia (tuberositas tibiae). The function of the patellar tendon is therefore to transfer the force exerted by the large anterior thigh muscle when the knee is extended.
The large anterior thigh muscle (musculus quadriceps femoris) consists of four muscles (m vastus lateralis, m vastus medialis, m vastus intermedius and m rectus femoris). The muscles all attach together on the upper edge of the kneecap. The patellar tendon (ligamentum patellae) connects the lower edge of the kneecap to the upper, anterior part of the tibia (tuberositas tibiae). The function of the patellar tendon is therefore to transfer the force exerted by the large anterior thigh muscle when the knee is extended.
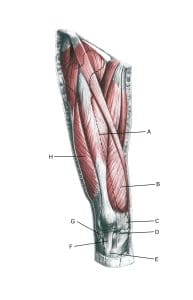
Knee from the front:
A. M. rectus femoris
B. M. vastus medialis
C. Retinaculum patellae mediale
D. Retinaculum patellae mediale
E. Tuberositas tibiae
F. Lig. Patellae
G. Retinaculum patellae laterale
H. M. vastus lateralis
Cause of the problem
Repetitive repetitive loading of the patellar tendon (jumping, kicking) causes microscopic ruptures at the patellar tendon attachment on the lower edge of the kneecap.
As the strain often continues despite the soreness, which initially subsides after warming up, a chronic ‘inflammation’ of the tendon gradually develops. In some cases, the symptoms occur at the tendon attachment from the anterior thigh muscle on the upper edge of the kneecap (‘upper jumper’s knee’).
Less commonly, the symptoms occur at the tendon attachment on the tibia (tuberositas tibia). Jumper’s knee is a very common overuse injury.
Symptoms
Initially, jumps and the like cause soreness at the lower edge of the kneecap. This pain subsides in the first weeks/months after warming up. If sports activity is continued, the pain increases and eventually makes sports activity impossible.
Examination
The diagnosis is usually made on general clinical examination, where there is localised pressure tenderness just below the lower pole of the patella. If there is any doubt about the diagnosis or lack of progress, an ultrasound scan should be performed early on to establish the diagnosis with certainty and assess the severity by detecting thickening of the tendon, blood vessel growth (Doppler activity) in the tendon, scar tissue formation, calcifications in the tendon and more.
View ultrasound scans of the kneecap and patellae.
Ultrasound scans can detect changes in jumper’s knee so early that there are no symptoms yet. This creates the opportunity to perform preventive training ( Fredberg U, Bolvig L, Andersen NT. 2008).
Treatment
The treatment of overuse jumper’s knee primarily consists of relief from the pain-inducing activity (jumping), stretching and slowly increasing strength training within the pain threshold. If treatment is started quickly, the injury can sometimes heal in a matter of weeks.
If the pain has been present for several months and ultrasound scans show thickening and changes in the patellar tendon, a rehabilitation programme over several months/half years is often required. Special emphasis is placed on strength training by activating the tendon while stretching it (eccentric training) or slow heavy strength training (Beyer R, et al. 2015) If relief and rehabilitation are not successful, rehabilitation can be considered supplemented with medical treatment in the form of arthritis pills, NSAIDs or injection of adrenal cortical hormone around the thickened part of the tendon.
As adrenal cortical hormone injection is always part of a long-term rehabilitation of a very severe, chronic tendon injury, it is crucial that the rehabilitation programme lasts several months (six months) to reduce the risk of relapses and ruptures, as the tendon will obviously not be able to withstand maximum load after a prolonged period of injury after only a short-term rehabilitation period.
Six months of rehabilitation before maximum load (jumping) is allowed is not unusual. See general, chronic tendonitis.
If rehabilitation and medical treatment are unsuccessful, surgical treatment may be considered. After surgery, about ¾ can return to sport at the same level (Cognetti DJ, et al. 2023).
Bandage
Some people find that applying tape or another bandage around the shinbone just below the kneecap can relieve the discomfort, See tape.
Complications
If no progress is made, you need to consider whether the diagnosis is correct or if complications have arisen.
In particular, the following should be considered:
