Anatomy
The bones of the knee joint include the femur (thigh bone), tibia (shin bone) and patella (kneecap). There is also a small joint between the tibia and fibula (fibula). The knee joint is reinforced by a joint capsule that is laterally reinforced with an external and internal collateral ligament (ligamentum collaterale laterale (LCL) and ligamentum collaterale mediale (MCL)). Inside the knee are two ligaments, the anterior and posterior cruciate ligaments (ligamentum cruciatum anterius (ACL) and ligamentum cruciatum posterius (PCL)).
Knee joint from the front:
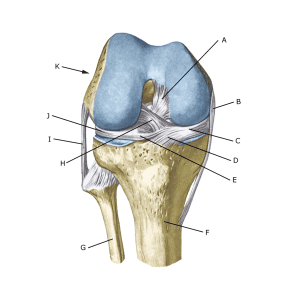 A. Ligamentum cruciatum posterius (Posterior cruciate ligament)
A. Ligamentum cruciatum posterius (Posterior cruciate ligament)
B. Ligamentum collaterale mediale/tibiale (Inner collateral ligament
C. Meniscus medialis (Inner meniscus)
D. Insertio anterior menisci medialis
E. Ligamentum transversum genus
F. Tibiae
G. Fibulae
H. Ligamentum cruciatum anterius (Anterior cruciate ligament)
I. Ligamentum collaterale laterale/fibulare (External collateral ligaments)
J. Meniscus lateralis (Outer meniscus)
K. Femur
Cause of the problem
ACL tears usually occur without contact with an opponent, where the athlete slows down and changes direction with greater weight on a slightly bent knee, for example in handball and football. Anterior cruciate ligament ruptures are most common in athletes and are far more common in women than in men and particularly common in female handball and football players. It is possible to reduce the risk of ACL injury with a simple preventive training programme (Myklebust G. et al., 2003), including Nordic Hamstring exercises, which are also included in current rehabilitation programmes (Chen JW et al., 2023)
Symptoms
Usually a pop is heard or felt and further sports activity must be cancelled. The knee swells within the first few hours, after which the knee cannot fully bend. Subsequently, you can often feel the leg giving way (knee failure).
Examination
If you suspect a total or partial rupture of the cruciate ligaments, you should see a doctor (emergency room) immediately to make a diagnosis. The doctor can perform various knee tests (anterior drawer laxity, Lachmann, Pivot shift) to examine the stability of the knee.
Be aware that looseness in the knee can often only be detected after 1-2 weeks. If the swelling occurs after an acute injury and a diagnosis cannot be made, the knee should be re-examined 2 weeks later to avoid overlooking an ACL injury, which can be difficult to diagnose in the acute stage. The ACL tear can be seen on MRI scans, where bone bruise (fluid inside the bone) can often be seen and 50% have meniscus lesions in an ACL tear.
X-rays should be taken to rule out tearing of the attachment. Bleeding at the anterior cruciate ligament attachment can be seen on ultrasound scans in the first few weeks as an indirect sign of rupture.
See ultrasound scan of torn anterior cruciate ligament
Treatment
Neuromuscular and strength training programmes can improve the functional stability of the knee, and almost half of those with a torn ACL do not undergo surgery. The majority of high-level athletes or in sports with rapid changes in direction (handball, football, basketball or badminton) are usually offered surgical reconstruction of the ACL (Filbay SR, Grindem H. 2019), although surgery has not been proven to be superior to rehabilitation in various studies (Mowbray MAS, Ireland J.2022, Rodriguez K, et al. 2021). There are different surgical methods including ACL suturing or ACL replacement (Shen Z, et al. 2022).
Acute surgery where the knee is still swollen with blood in the joint can lead to reduced mobility after surgery. Therefore, it is usually recommended that the knee is elevated and mobility is regained before surgery. Treatment of ACL injuries in athletes under the age of 16 is a highly specialised task due to consideration of the growth plate (epiphysis) and should be referred to a specialist department. The prognosis is dependent on other concomitant knee injuries (Petersen W, et al. 2023)
Complications
If no progress is made, you need to consider various complications of the surgery:
In particular, the following should be considered:
- Fluid accumulation in the joint
- Outer collateral ligament rupture
- Inner collateral ligament rupture
- Rupture of the posterior cruciate ligament
- Meniscus lesion
- Cartilage damage on the knee cap
In cases where the patellar tendon has been used as a new cruciate ligament, ‘inflammation’ is frequently seen where the patellar tendon has been removed. Approximately 60% of elite athletes return to their pre-injury level.
Specifically
As there is a risk of permanent damage, the injury should be reported to your insurance company.
