Anatomy
The pelvis consists of 2 halves, joined at the back by the sacrum and at the front by the pubic symphysis. The symphysis is not a true joint but consists of fibrous cartilage (fibrocartilago) that connects the two pubic bones. Only small rocking movements are possible. The abdominal muscle (M rectus abdominis) attaches to the pubic bone. The inner thigh muscles (e.g. M adductor longus) attach to the groin just below the pubic bone.
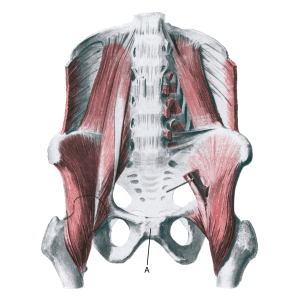
The pubic joint:
A. Symphysis pubica
Cause
Repeated repetitive repetitive (over)strain causes an (inflammation) of the pubic symphysis pubis joint, whereby the joint can become loose, allowing the two halves of the pelvis to move slightly in relation to each other under heavy loads.
This is especially common in sports characterised by fast running activity with sudden changes of direction (football, ice hockey) and long-distance runners. Symptoms can be triggered by trauma (e.g. ski jumps).
Inflammation of the pubic joint is common in pregnant women.
Symptoms
Pain around the pubic joint, abdominal attachment to the pubic bone and groin. Aggravated by asymmetrical loads (e.g. jumping on one leg).
Examination
Diagnosis is usually made by general clinical examination. There will often be tenderness at the pubic joint (direct and indirect). The examinations can be supplemented with X-ray, CT, MRI or ultrasound scans.
Treatment
Inflammation of the shin joint is often preceded by long-term groin pain where the strain has continued despite pain. A rehabilitation period is often required, which in severe cases can last up to a year. It is therefore crucial to start treatment as soon as possible without continuing the triggering sporting activity.
Treatment primarily involves relief from pain-inducing activity and then slowly increasing strength training of the muscles around the pubic joint (abdomen, groin), pelvis and lower back within the pain threshold.
If rehabilitation is unsuccessful, medical treatment may be considered in the form of NSAID or injection of adrenal cortex hormone into the pubic joint (Byrne CA, et al. 2017). Surgery is usually not indicated.
Complications
If the progression is not smooth, you should consider whether the diagnosis is correct
In particular, the following should be considered:
- Inflammation of the adductor of the thigh
- Fluid accumulation in the joint
- Degenerative arthritis
- Brupture of the superficial hip flexor
- Rupture of the deep hip flexor
- Inner snapping hip
- Fatigue fracture of the femoral neck
- Inguinal hernia
- Sportsman’s hernia
- Inflammation of the abdominal muscle at the point of attachment on the pubic bone
- Bursitis on the front of the hip joint
- Nerve entrapment
